September 8, 2025
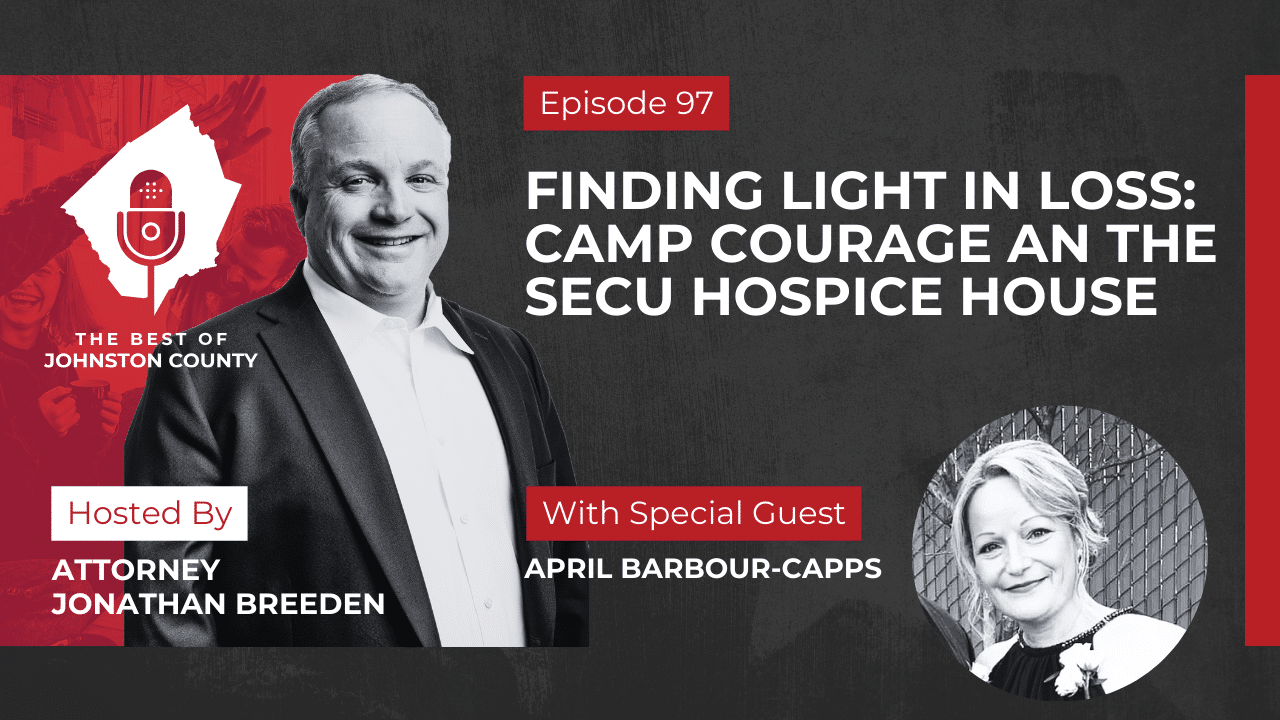
Finding Light in Loss: Camp Courage and the SECU Hospice House
Jonathan Breeden: [00:00:00] On this week’s episode of The Best of Johnston County Podcast. Our guest is April Barbour-Capps of the SECU Hospice House in Johnston County. We talked to her a little bit about Camp Courage, which is a free camp for children ages six to 17 that are going through grief and it’s a tremendous asset for this community where children can get together and learn that they’re not alone. We also talked her a little bit about the evolution of the SECU Hospice House in Smithfield, how much it costs and how your family can use such a great asset in this community. So if you’re interested in general things about grief or this Camp Courage for to help grieving children, listen in.
Welcome to another episode of Best of Johnston County, brought to you by Breeden Law Office. Our host, Jonathan Breeden, an experienced family lawyer with a deep connection to the community, is ready to take you on a journey through the area that he has called home for over 20 years. Whether it’s a deep dive into the love locals have for the [00:01:00] county or unraveling the complexities of family law, Best of Johnston County presents an authentic slice of this unique community.
Jonathan Breeden: Hello and welcome to another edition of the best of Johnston County Podcast. I’m your host, Jonathan Breeden, and on this week’s episode we have April Barbour-Capps, who is a social worker and bereavement coordinator for UNC Health Johnston, and helps run the SECU Hospice House in Smithfield and she’s here to talk to us a little bit about Camp Courage, which is coming up on September 27th, 2025, which is a camp for children between the ages of 6 and 17 that they can go to and do fun activities and meet with people that are trained and, and, bereavement and loss so that they can help process some of the losses they may have had.
And we’re gonna talk a little bit about hospice in general and the SECU Hospice House and the services it provides. One thing that I have learned as we got ready to take this is there’s lots of hospice providers in Johnston [00:02:00] County and not just one. So we’re gonna talk a little bit about that as well.
Before we get to that, I’d like to ask you to like, follow, subscribe to this podcast wherever you see it, whether it be on Apple, YouTube, Spotify, TikTok, LinkedIn, or any of the other social media channels of The Best Johnston County Podcast. The Best Johnston County Podcast comes out every single Monday and has now for almost two years.
So go back and listen to some of our previous guests. We’ve had most of the county commissioners, we’ve had a lot of elected officials, small business owners county manager, Rick Hester county Parks Director, Adrian O’Neal. Lot of great people have been on this podcast. If you love Johnston County as much as I do.
This is the podcast for you. So be listing in, go back and list some of the previous episodes. It’s a lot of fun. We enjoy bringing it to you, and I think you’ll learn a lot. Welcome April.
April Barbour-Capps: Thank you.
Jonathan Breeden: I think I got the title right?
April Barbour-Capps: You did.
Jonathan Breeden: I had to practice before we started.
April Barbour-Capps: You did? You did.
Jonathan Breeden: Okay. I got, it’s a. That’s a lot. That’s a, that’s a long title. So anyway, I was trying to, I get these titles mixed up, but at least, and I didn’t get, I didn’t call you Capps Barbour.
April Barbour-Capps: You [00:03:00] didn’t, you did good.
Jonathan Breeden: I was gonna do that too. So it’s Barbour-Capps. So anyway all right. So, state your name and, and what you do.
April Barbour-Capps: Yes. So I’m April Barbour-Capps. I’m a social worker and the bereavement coordinator for SECU Hospice House and our home hospice program, which is UNC Health, Johnston, home Care and Hospice. So I’m the social worker and bereavement coordinator for both of those.
Jonathan Breeden: Okay. And what does that mean?
April Barbour-Capps: Yeah, so good question. So part of a care team, hospice in general is a team of individuals, of course. So social work is one component of that interdisciplinary team. And as part of the conditions of participation for Medicare, we have to two offer bereavement services for 13 months following a hospice patient’s death. But even more so, we offer community bereavement services as part of those conditions of participation for Medicare, and a lot of our community doesn’t know that.
But we offer those services just as we would for a hospice family that we’ve served. We offer those for anyone in our [00:04:00] community who’s lost a loved one. So we have adult grief support groups that we run on a regular basis. First Wednesday night of every month over at the medical mall, we do an adult grief support group called Seasons of Grief. Myself and our other social worker Heidi Erickson, who’s a licensed clinical social worker, we run that group together. And then. like I said, we, we, her and I also split seeing all the patients on the inpatient side in the hospice house, as well as our home hospice patients
as well. Offering just supportive services, resources short-term counseling, you know, all the support
that that comes from hospice.
Jonathan Breeden: Okay, so how did you end up in this? I know you’re from Four Oaks, you went to Campbell, so how did you get started getting into, I mean social
work and then in the bereavement business?
April Barbour-Capps: Yeah,
so I was going to be a journalism major. That was going to be what I wanted to do. I lost a brother in 1989 when I was, between sophomore and junior year [00:05:00] of high school South Johnston. and my brother was killed in a tragic car accident directly in front of the high school that I would keep attending for the next bit. So that changed the trajectory of what I realized I wanted to do because I then realized there were no resources in our county for grief and loss, hardly any. There were no resources for my parents who were grieving the loss of a child, no resources for siblings grieving the loss of a sibling. There just weren’t resources. And from there I decided that grief and loss would be, there would be resources at some point. So that is the direction I took. I went and got my undergrad from Campbell in social work and then went straight back and got my
graduate degree in community
counseling.
Jonathan Breeden: Okay. I got you. And you’ve been with Johnston Memorial Hospital, now UNC
Health for 30 years.
April Barbour-Capps: 30 years. 30 years. I was an intern there in my undergrad. and immediately
finished my undergrad. They hired me and I have been there pretty much either full [00:06:00] or part-time ever since.
Jonathan Breeden: Okay. And Have you been doing bereavement the whole time?
April Barbour-Capps: For the most part, yes. When I was hired I was hired in initially a discharge planning position, but that was brief. I immediately transitioned over to our home hospice. ’cause at the time we didn’t have hospice house then. So worked our home hospice side, pretty much through the hospital of fluctuated between case management.
Home hospice and the inpatient hospice the entire time I’ve been at Johnston.
Jonathan Breeden: Okay. Alright. Well, I mean that’s, that’s a long time and you’ve seen a lot of change in that hospital.
April Barbour-Capps: Yes, yes.
Jonathan Breeden: From a small community hospital in rural area,
April Barbour-Capps: yes.
Jonathan Breeden: To being part of one of the larger hospital systems in this part of the country.
April Barbour-Capps: Yeah. The growth has been
amazing. Amazing to watch
Jonathan Breeden: you enjoy, working with the UNC Health team now.
April Barbour-Capps: I do.
Jonathan Breeden: And, and the resources they brought,
April Barbour-Capps: I do. Even though it’s a larger system, it’s, there is still a sense of community because so many of the employees of Johnston are still local people who still enjoy serving their own community, which is what’s kept me here that long, is I enjoy serving the [00:07:00] people in
my own community.
Jonathan Breeden: Well, that’s cool.
April Barbour-Capps: Yeah.
Jonathan Breeden: So, let’s talk a little bit about, so Camp Courage is a camp for children that are going through grief. Where did that ideal come
from? How does it work?
April Barbour-Capps: Yeah, so, one of the social workers previously at the Hospice House developed the concept for camp Courage. And I wanna say we did our first one back in 20, I wanna say 2011. 2014 was our first camp courage. hospice house was built
in 2011.
So out of that group, recognizing that there’s not a lot of grief resources for children in our county and there’s not and so especially not resources that are free of charge, Camp Courage is made possible through UNC through our hospital foundation, through donations from our community, specifically for the hospice fund and camp courage.
And so from that grew this day program that we dedicate to helping children and youth, learn how to cope better, learn better coping skills, be around other youth who have experienced a similar [00:08:00] loss. And you know, I tell people all the time, that’s where the magic happens, is putting kids with other kids who have experienced similar losses and they realize, Hey, I’m not the only person going through this. And it’s an amazing day. We have volunteers from. Our
public safety. We have volunteers from other therapists in our community, from school counselors, from our own social workers and counselors and our hospice volunteers. It’s just a a great team of people, that pull together that day to, to put on this program
for children. It occurs outdoors, so we always say extra pairs for great weather. We’ve never been rained out. Knock on wood. But we use nature and we use outdoors as part of the way to help children learn how to
navigate grief.
Jonathan Breeden: So what are some things that everybody can do to navigate grief better, whether it be a child or an adult?
April Barbour-Capps: Yeah, so I would definitely say finding what brings you some peace and joy. So we teach kids, for example, and adults about coping [00:09:00] strategies and skills. So if it’s listening to music, if it’s journaling, if it’s taking a walk outside, you know, part of the stations that we do for camp courage involve drums and drumming and musical instruments.
And so just trying to tap into any and every aspect that may bring you peace, may bring you joy, may create a diversion for you when you’re struggling or stressed about grief and also opening the door to make it okay to talk about. Nobody wants to talk about grief and death. Nobody wants to talk about it but it is necessary and it also helps with coping to open that door to say it’s okay to have a conversation about death and dying and about grief and loss, and realize that other people are walking that path too.
Jonathan Breeden: Yeah. Well, and I, I think that’s important. ’cause I think a lot of people, they
wanna bottle it up.
April Barbour-Capps: Mm-hmm.
Jonathan Breeden: They wanna try to deal with it themselves. They, they get out of their normal routine, they. They separate from their friends. Maybe they don’t go back to work or they go back to [00:10:00] work, they’re going through the motions and, and, and that’s not going to
help the situation, I don’t believe.
April Barbour-Capps: No. We tell people all the time. You can tuck it back. You absolutely can tuck grief back. You can tuck it back, but at some point it will rise to the surface. And if you’ve tucked it back, when it does rise to the surface, it’ll be like a volcano erupting versus. Having
faced it head on we tell people there’s only one way through grief and it’s straight through the middle of it.
You can’t go around it, you can’t go under it. You can’t go over it. There is no
way except straight through the middle.
Jonathan Breeden: Yeah. And you know, well, you know, sometimes we have to deal with death in family law because I mean, sometimes our clients. Kill themselves.
April Barbour-Capps: Sure, sure.
Jonathan Breeden: Or they kill their partners.
Or they kill their children.
I mean, I’ve, I’ve, had to go through all of that. Yeah. And that was a unique thing for me, particularly as a young attorney when it first started happening, because mm-hmm. I’d been representing these people, I was trying to do what I could for ’em, and then all of a sudden they’re [00:11:00] gone and the first thing I
wanted to do is, okay. Did I do something wrong?
April Barbour-Capps: Mm-hmm.
Jonathan Breeden: Could, could I have handled this case? Yeah. Differently? Could I have done something? Yeah. And ultimately I couldn’t. Right? Yeah. Like I was just a lawyer. I was in their lives for some short period of time. Right. you know, I didn’t cause it, but I, you know, I did want to sort of. initially blame myself when it was happening.
April Barbour-Capps: Sure.
Jonathan Breeden: I was a young, young man. I didn’t quite understand it, but you know, I learned to process it and,
and deal
with it and realized that that, that I didn’t do it right. Yeah. Like these people had whatever problems they had and it is, and you know, we have to work our young attorneys, you know, fortunately we had
a, we had a, you know, not too long ago where we had some you know, family members get killed in a domestic violence situation. And it, it’s a lot.
April Barbour-Capps: Sure.
Jonathan Breeden: It’s, and enough to be able to. To process. If you wanna do family law, you gotta get used to it. You know what I mean? Right. The other thing we see here is, I don’t know, it’s interesting is
that I think a divorce causes grief, right? Like I think you think this,
April Barbour-Capps: it’s a loss
Jonathan Breeden: sort of a,
April Barbour-Capps: it’s a loss.
Jonathan Breeden: It’s a loss. It’s a significant loss. Yes. Maybe not the loss of
a parent, but it’s right up [00:12:00] there is the stress thing. And so I’ve watched people over the 25 years I’ve been doing this. Go through those sort of stages of grief as we’re trying to represent them. You know, and, and I don’t know ’em all, I’m not a social worker, but I know that it’s a good place when you’ve processed it and sort of dealt with it.
I don’t know that’s the last phase or what you call it, but like You’re over it or whatever.
April Barbour-Capps: Yeah.
Jonathan Breeden: Talk a little bit about the phases and how they work.
April Barbour-Capps: Yep. So I’ll definitely say I’m glad you used that terminology. ’cause we always tell folks there is no over it
Jonathan Breeden: Okay.
April Barbour-Capps: There’s a carrying it with
you. And a carrying it with you in a more healthy manner. Like that’s the goal of grief is to be able to remember, but with less pain than what you are experiencing. In the moment,
we often describe it as like a backpack. And at first grief is really heavy like someone’s put rocks in it and it’s just super hairy heavy, and you know that you’re carrying it with you. You feel it every single day. But over time, as you allow yourself to process the grief, maybe access resources and get the support you need, it’s like a rock comes out here and there and you still [00:13:00] know you’re wearing the backpack, but it’s lighter. And that’s sort of how no, you’re wearing the backpack, but it’s lighter.
And that’s use is, it just becomes a lighter experience if, but definitely around since the concept of hospice, since the Middle Ages. so comfort, care, dignity, you know, quality of life. Those things have been around quite some time, but, you know, with, with grief itself, those stages are so fluid. Like I tell people, you, Elizabeth Cooper Ross was one of the pioneers in, in talking about those stages, you know, bargaining and anger and acceptance and denial. The thing about those stages is they’re not pretty and you don’t go through one and then two, and then three, and then four. You
may go through four, back up to one, two, then to five, and then back up to one again. It’s very fluid as you grieve. You will not go through those stages pretty, it won’t be like textbook.
you will fluidly go in and out of those stages throughout grief. Okay?
One day you may be angry. [00:14:00] One day you may be back in complete shock. One day you may be more accepting of the loss. It, it truly does come and go through grief.
Jonathan Breeden: That is interesting and it is interesting, you know, in, in a divorce context where, you know, a lot of times, you know, we’re, we’re talking to a a, you know, if we’re talking to the spouse that wants a divorce, they have gone through those stages while they’re in it wants a divorce. They have gone through those stages while they’re, whether they should have gone going through it. Right.
Which means we could end up being
Jonathan Breeden: the target of some of the, the anger. mm-hmm
and frustration.
April Barbour-Capps: Mm-hmm.
Jonathan Breeden: That is part of the grieving process of the loss of the relationship.
April Barbour-Capps: Yeah.
Jonathan Breeden: That we didn’t have anything to do with
April Barbour-Capps: Yeah. you know, so.
Absolutely.
Jonathan Breeden: So we do, we do you, you’re always cognizant of that right. Loss, I mean, loss is loss and
April Barbour-Capps: Yeah. But there are are multiple different kinds of losses,
Jonathan Breeden: correct
April Barbour-Capps: Absolutely. Multiple different kinds.
Jonathan Breeden: Right.
Have family law questions? Need guidance to navigate legal challenges? The compassionate team at Breeden Law Office is here to help. [00:15:00] Visit us at www. breedenfirm. com for practical advice, resources, or to book a consultation. Remember, when life gets messy, you don’t have to face it alone.
Jonathan Breeden: Well, let’s talk a little bit about the SECU, State Employees Credit Unit, hospice house SECU Anyway, Hospice House it’s a place where you can go. We were talking, I did go to the ribbon cutting in like 2011.
It was absolutely amazing place. I did not know places like that existed. It did not feel like I was in a nursing home or a medical facility at all. fortunately I’ve not been back since the ribbon cutting in 2011 has a chapel. I mean, it was just, it does really nice.
So talk about what it’s purpose is. How people use it. Does it cost?
April Barbour-Capps: Yeah, so it’s an 18 bed facility. All private rooms, private bathroom, private room beautiful large windows. I mean, attention was paid to detail here to try to make it not look. Institutional in any way. Of course we have things that we have to [00:16:00] have as, as providing medical equipment and such, but great attention was paid to make it not look institutional. The rooms very much look homelike. To give an example, like, you know, we have oxygen just like the hospital does through the wall, but it’s in a cabinet. So it’s not just in plain view so that you know, you’re not seeing things that are constantly reminding you or scary for kids that are visiting the hospice house.
We try to keep those things camouflaged and make it look more like a home. Your, your bedroom at home. We do still have an interfaith chapel. We have a children’s playroom. We have a large family kitchen where families can come and, and have a meal together and if their loved one’s able to get outta bed and we’re able to get them in a wheelchair, they can go have, we’ve had.
Families throw birthday parties for their loved one in that big family kitchen. We have outdoor patio areas where families can take, you know, their loved one outside, or families can go outside and just get a break. We have meditation rooms where families can just go and take a break from the, the room itself or the, the stress of [00:17:00] being in the room and, and watching their loved one die.
Those meditation rooms are designed to just provide peace and comfort and a quiet time, a place for them to, to just be, our staff, utilize that some too, because as you would imagine, taking care of dying people every day is not an easy job. But it is an important one and, and we’re rewarded in other ways not address rehearsal.
As I say about hospice. We get one chance. There’s no do-overs. You get one opportunity to get it right for the patient and the family, and so staff are very committed to trying to make sure it’s as positive of an energy as possible when we’re dealing with these patients and families. No one likes to talk about hospice.
No one likes to talk about death and dying, but the fact that we’ve received you in our facility means that you are faced with that. You and I spoke before the camera was on that people do graduate from hospice, so it happens.
Jonathan Breeden: We both have a mutual friend who graduated from hospice. It happens, right? It does. It uh, It it does. Yeah. And, uh that, that’s, that’s great too. Yeah. You know [00:18:00] what I mean? And
April Barbour-Capps: hospice provides care for lots of different diagnoses. So a lot of times we don’t see the graduation and care with our cancer diagnoses because that typically takes. The, the decline. But Alzheimer’s disease, sometimes instate heart disease or endstage liver disease, sometimes we think, or maybe they’ve had an event, a hospitalization, and maybe they’ve declined in their eating and their drinking and we think, okay, this is it. And then they come to us and we give such great tender loving and care that they wind up improving and getting better. And then we have to help them get to the next place of care. That’s, whether That’s, home or rehab or whatever that might be. And we help them get to that next place. We don’t just tell families, you know great see you later. We help them find what that next level of care is. But we do have people that graduate. We do, right.
Jonathan Breeden: Well, and, and, and to stay in the hospital’s house, you said the cost is $95 a day,
April Barbour-Capps: so that’s the out of pocket for what room and board we call it. Okay. That’s the part that Medicare, so Medicare, Medicaid, and [00:19:00] many of the private insurances will pay for the other services. What it typically won’t cover is that room and board cost, because we are considered like a specialty care center. So that $95 a day is, the out-of-pocket cost for the residential level of care. Patients that we have, hospice patients that we have that are experiencing some sort of out of control symptoms, out of control, pain, maybe out of control, nausea, and are requiring IV medications that we can’t necessarily do at home. Medicare, Medicaid, private insurance, those will often pay for those days with no out of pocket because it’s a considered a more acute level of care and we’re providing something we can’t do in the home environment. So it couldn’t be provided any other place. Okay. Except a, a clinical setting. and then we have respite stays for our home hospice patients and even other hospice agencies. Where patients can come for five days and let families take a vacation, or families take a break. Or often we’ve had families need to get a knee replacement, or maybe they’re sick with the flu, and we just need somewhere the patient to be safe and [00:20:00] receive care until the family is back where they can care for their loved ones. So they’ll come in for that five days, Medicare pays for that and then they’ll transition back home.
Jonathan Breeden: Right. Well, the last question I’ll ask you is there’s more than one hospice provider in Johnston County, right? Yes, there are. And the hospital is one of them.
Yes. It is. Or U UNC Health is one,
April Barbour-Capps: correct? It is the best one.
Jonathan Breeden: It’s the best one, right? It’s the best one. Because it employs April That’s
April Barbour-Capps: right. It is the, no, it’s the best one because it’s the best one. It’s the best one, right. So a a great question. Yes, there are multiple agencies that come into the county that provide home hospice services. None of those other agencies own or are affiliated with the Hospice House? the Hospice House? is owned by UNC Health Johnston. Okay. So our home hospice and the inpatient unit are under the same umbrella. And so one of the biggest benefits I will say, that sets us aside. So say we admit a patient to our home hospice program and things start to change, the care becomes too much for a family and they’re needing to transition to the inpatient side for care for safety. So [00:21:00] we often are full. And so say we’ve got one bed open and three other referrals, some of which are from another hospice agency trying to get their person placed. Our bed goes to our agency because it’s our agency. They’re already our patient. Already your patient, side. And so we have to provide that service to our patient. And so being affiliated with our home agency also makes you affiliated with our inpatient side. and it’s a benefit.
Jonathan Breeden: So how could people reach out to you and find out about Camp Courage? Yeah, which is coming up real soon. You do it once a year?
April Barbour-Capps: Once a year. September 27th at Sonlight Farms in Kinley and you can find information on the hospital website. If you are interested in registering your child or getting more information, can call me directly.
Jonathan Breeden: Okay.
April Barbour-Capps: ( 919) 209-3478 or call the Hospice House main number 9 1 9 2 0 9 5100. But anyone there can give you more detailed information. But we still have openings, so we would love to reach any and every [00:22:00] kid or youth in our county, we actually get kids coming from Wake County, from New Hanover County, which is why I say there’s not enough resources for children, right? Because we get people from so many other places looking for that resource for their, that’s great, good job.
Jonathan Breeden: So born and raised in Johnson County, been here your whole life. You said you’ve only moved a hundred feet. I know. Three times in a hundred feet each. times. time. Hundred feet of I know, right in For Oaks. What do you love most about Johnston County?
April Barbour-Capps: The sense of community, I would say. I was born and raised on a family farm. My dad was a farmer. The sense of community for Oak still has a huge sense of community. And even though Clayton and all its growth and some other places with all its growth, I still think that is something that sets us apart that most. Times you will find someone, you know? that’s true. Yeah. And I just feel like that sets us aside from some larger places. Well, that’s great.
Jonathan Breeden: Well, we’d like to thank April Barbour-Capps for being our guest on this week’s episode of The Best Johnston County Podcast.
If you would do us a favor, the, like, follow, or subscribe this podcast wherever you see it. Tag us in your [00:23:00] Instagram stories. Best of Johnston County. Uh, leave us, leave us post review. Make sure you subscribe wherever you’re seeing it should be made aware of. Future episode of The Best of Johnston County. Until next time, I’m your host, Jonathan Breeden.
That’s the end of today’s episode of Best of Johnston County, a show brought to you by the trusted team at Breeden Law Office. We thank you for joining us today and we look forward to sharing more interesting facets of this community next week. Every story, every viewpoint adds another thread to the rich tapestry of Johnston County.
If the legal aspects highlighted raised some questions, help is just around the corner at www. breedenfirm. com.
One of the things I love about hosting The Best of Johnston County Podcast is that it gives me the chance to highlight people who are doing meaningful work in our community. In this episode, I had the privilege of sitting down with April Barbour-Capps, a social worker and bereavement coordinator at the SECU Hospice House in Smithfield. What she shared with me about grief, healing, and community left a lasting impression.
Camp Courage: A Lifeline for Grieving Children
April told me about Camp Courage, a free day camp for kids ages 6 to 17 who are dealing with grief. It started back in 2014, after staff at the hospice recognized that there weren’t many resources for children in Johnston County who had lost someone they loved.
The camp is completely free, thanks to donations through the hospital foundation, and it’s designed to give kids a safe place to talk about their loss, learn coping strategies, and most importantly, realize they are not alone.
I loved hearing April describe the “magic” that happens when children who’ve gone through similar experiences sit together and say, “I’m not the only one.” The day includes activities like drumming, journaling, and outdoor play, all led by a team of volunteers: school counselors, therapists, social workers, hospice staff, and even public safety officers.
How We Carry Grief
April has spent more than 30 years walking with people through grief. She explained that it’s not something you “get over.” Instead, you learn to carry it differently. She compared it to a backpack full of heavy rocks, at first unbearable, but as time goes on, some of those rocks are lifted, and the load gets lighter.
She also reminded me that grief doesn’t follow a straight line. You may feel acceptance one day and find yourself back in shock or anger the next. That’s normal. What matters is finding ways to cope, whether through music, journaling, walking outside, or simply giving yourself permission to talk about loss.
I’ve seen this in my own work as a family lawyer. Sometimes the grief of divorce looks a lot like the grief of death. I’ve had clients who’ve taken their lives, or worse, harmed family members. Early in my career, I wondered if I could’ve done something differently. But I’ve come to accept that while I can walk with people for a time, I can’t carry their burdens for them. April’s words affirmed something I’ve long believed: loss is loss, and it deserves compassion.
Inside the SECU Hospice House
I still remember attending the ribbon cutting for the SECU Hospice House back in 2011. I was blown away by how different it felt from a hospital or nursing home. April described how intentionally it was designed: 18 private rooms, each with large windows and private bathrooms, with even the medical equipment tucked away in cabinets to reduce the “clinical” feel.
There’s a family kitchen where loved ones can share meals or even throw birthday parties, meditation rooms for quiet reflection, and a children’s playroom. Families can sit outside on the patio or take a breath of fresh air when they need it.
The cost is $95 a day for room and board, but most of the medical care is covered by Medicare, Medicaid, or private insurance. Families can also use the Hospice House for short respite stays, giving caregivers a few days of rest while their loved ones are cared for. And sometimes, patients even “graduate” from hospice, especially those with conditions like heart disease or Alzheimer’s who improve under attentive care.
“Hospice isn’t a dress rehearsal,” April told me. “We get one chance, no do-overs.” Hearing the pride in her voice as she described her team’s commitment made me grateful for the work being done right here in Johnston County.
Community Roots
April’s commitment to this work is deeply personal. She lost her brother in a car accident as a teenager, and that tragedy led her into social work. She’s been with Johnston Memorial Hospital, now UNC Health Johnston, for three decades. Born and raised in Four Oaks, she’s never lived more than 300 feet from the family farm where she grew up.
What’s kept her here all this time? “Serving the people in my own community,” she told me. And that’s exactly what she’s doing, every single day.
Learn More
Camp Courage will take place on September 27, 2025, at Sonlight Farms in Kenly. If you’d like to register your child or learn more about grief support services, call the SECU Hospice House at (919) 209-5100 or reach April directly at (919) 209-3478.
Conversations like this remind me why I love hosting The Best of Johnston County Podcast. Every week, I get to share stories of people like April, neighbors who are working tirelessly to make our community stronger, kinder, and more connected.
AND MORE TOPICS COVERED IN THE FULL INTERVIEW!!! You can check that out and subscribe to YouTube.
Connect with April Barbour-Capps:
- Hospice House Phone: (919) 209-5100
- Personal Phone: (919) 209-3478
Connect with Jonathan Breeden:
- Website: https://www.breedenfirm.com/
- Phone Number: Call (919) 726-0578
- Podcast: https://breedenlawpodcast.com/
- YouTube: https://www.youtube.com/@BestofJoCoPodcast




